Fresh perspectives on age-old benefits questions

Our recent webinar, Building Your Benefits Business Case: Get Seen by the C-Suite, prompted some thought-provoking, valuable conversations between the three CEOs on our panel. Rajeev Singh, Chris Todd, and Jon Shanahan formed the perfect cast to discuss how HR professionals can work best with their C-suite leaders to do right by their employees.
Their conversation, now available via on-demand recording, covered many topics, including one of the most pressing ones for employers this year—addressing employees’ mental health.
Employers can use mental health support to bridge the empathy gap
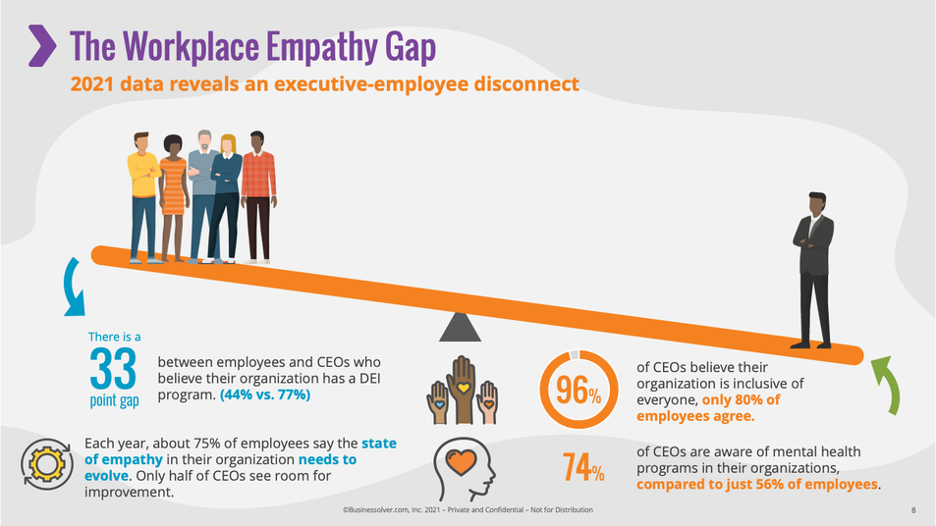
One thing that stands out in the graphic above is that according to Businessolver’s 2021 State of Workplace Empathy data, 74% of CEOs are aware of mental health programs, yet only 56% of employees say they are aware. This discrepancy prompts immediate questions, and there was no one better to answer than Raj. Raj is the CEO of Accolade, a company focused on helping other organizations engage their employees to help them and their families live healthier lives. Accolade does that by giving employees and their families a care team that includes a primary care physician, a mental health specialist, and people who can run down their health care claims; that care team becomes the front door to all things related to health care and benefits.
However, not every employee has an Accolade care team—particularly when it comes to addressing mental health, which has emerged during the pandemic as a critical issue for employers nationwide. Raj acknowledged that employees’ discomfort with questions like, “Do I want to seek help from my employer when I'm wrestling with depression, anxiety, or things like substance abuse where the need for privacy is extraordinary?”
“Beyond that,” he continued, “we also have to acknowledge that employees are underserved by traditional EAP programs.”
“Oftentimes what people are getting when they call into those EAP programs is, ‘Hey, here's a list of 15 providers in your area. We have no idea whether they're accepting patients. We have no idea whether they're really still in network or how much they're going to charge. But hey, give them a call and see how you do.’ And there are legions of stories of people [unsuccessfully using EAPs] to find mental health help for their families.”
That’s not to say employers are to blame, though, Raj assured the audience. “It's very feasible that the employer believes they've contracted in a way that solves this problem for their people, meaning the employer is well-intentioned. And yet the reality on the ground is those phone calls are going to show that 14 of those providers aren't accepting patients, and the one that is accepting new patients won’t see them for another three months and may not accept their insurance anymore.”
“This is one of the more profound crises in the country right now, but I think it's one of the more profound opportunities we have to engage employees. When [benefits leaders] can solve that problem for them and for their families, we've met them in a moment of need with a highly personalized solution that'll change their relationship with [their employer].”
Check out the on-demand webinar recording, transcript, and slide deck for all can’t-miss insights from the entire hour—including the one thing each CEO on our panel said you can do to improve your effectiveness within your organization below.



